When children fall on a playground, they’re up again in a minute or two with just a kiss to make it better. But the risks and consequences of falls in the elderly become more serious with each passing year.
As we age, our reflexes grow slower and we lose our ability to react quickly when unexpected trips, stumbles, and unsteadiness occur. At the same time, our bones become increasingly brittle and porous. Skin becomes thinner and more fragile. Muscle mass decreases without regular weight-bearing exercise. We lose the physical conditioning that helps us balance, walk steadily, and recover from wobbles. Nerves in the feet may grow less sensitive. Prescription and nonprescription medications may dull the senses. Vision and hearing deficits can make us less aware of hazards.
Thankfully, we know a great deal about how to prevent falls.
These factors and more can add up to serious injuries, devastating recovery costs, and permanent threat to independence.
Thankfully, we know a great deal about how to prevent falls in the elderly, how to detect and respond to them when they do occur, and how to quickly get help to older people who have fallen to ensure they get the help they need to recover as quickly and completely as possible, so they can return to independent living.
Injuries and deaths due to falls in the elderly
The government keeps track of statistics about visits to emergency departments and hospitals. Because of this, we know a lot about who falls, what happens to people after they fall, and what kinds of fall injuries are most common.
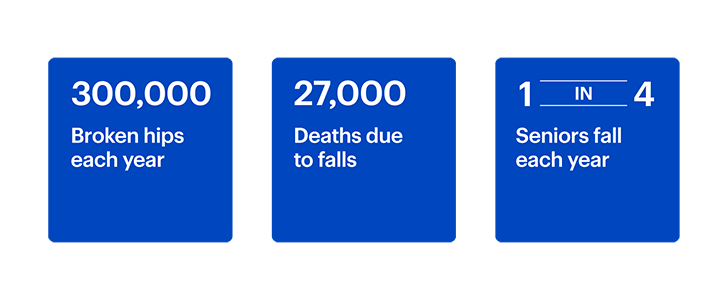
People over 65 who fell: One in four older adults reported a fall over a one-year period; not all told their physicians.
Hip fractures: Of 300,00 broken hips annually, 95% resulted from falls. Most broken hips from falls affect women (70-75%), and most of those occur from sideways falls.
Head injuries: From 2007 to 2013, the rate of brain injuries from falls in the elderly increased 76 percent. Traumatic brain injuries (concussions) account for about 30 percent of all fall-related deaths. Head injuries are the most common fall-related injuries in men.
Broken bones and other injuries: Broken wrists, arms, legs, vertebrae, and ankles are among other common injuries due to slips and falls on wet floors or pavement, slips off of curbs and falls down stairs. An estimated one in five falls results in breaks to bones other than the hip. Some estimates place the rate of broken bones due to falls in older people as high as 87%. Other serious injuries associated include skin tears and associated bleeding (which can be quite dangerous for people on blood thinners) and secondary complications associated with waiting a long time for help, such as dehydration, kidney failure, and pressure ulcers.
Deaths: 39,000 deaths due to falls in the elderly were reported in 2021. And the U.S. Centers for Disease Control (CDC) expects that number to keep rising steadily until it hits seven per hour by the year 2030.
The cost of falls in the elderly
The costs of falls and the injuries they cause are significant for those who experience them as well as their families, friends, and communities, creating both fiscal and psychological burdens for older people and communities.
With more than 800,000 annual patient hospitalizations due to falls in the elderly (most due to broken hips or head injuries) the road to recovery can be long, difficult, expensive, and daunting.
Researchers calculate that patients, families, and insurance companies paid $50 billion in direct costs associated with falls in the elderly in 2013. (Direct costs are those associated with hospital stays, doctors and other medical professionals, long-term rehabilitation stays after hospitalization before going home, insurance processing, and additional community-based services.)
...the average cost of a fall-related hospitalization and rehabilitation is $35,000.
Medical costs: While there is no such thing as a “typical” fall because the types and severity of fall injuries vary so widely, researchers have calculated the average cost of a fall-related hospitalization and rehabilitation is $35,000. Medicare paid approximately 78% of this cost more than a decade ago. That leaves a substantial monetary burden for older people and their caregivers living within modest means.
Psychological costs: Perhaps the most devastating costs of falls, however, are not financial. The social and psychological after-effects of falls are psychological and emotional. Falls requiring medical care frequently generate fear of another fall; this can prompt people to limit their everyday mobility, physical activity, and social activity, which leads to further loss of physical conditioning.
Thus, fear of falling can lead to a downward psychological and physical spiral with real consequences, including further deterioration, depression, social isolation and loneliness. Such costs are not merely emotional in nature: Loneliness and limited social interaction have been linked to a higher risk of death in older adults as young as 52 years of age.
The role of fall detection systems in quick response and recovery from falls in the elderly
In a worst-case scenario, if and when a fall happens, how quickly help arrives is critical to the odds for a speedy, easy recovery and the ability to return to independent living.
Response time is critical. “Lie time,” or the duration of time spent alone helpless after a fall, is a direct predictor of the likelihood of recovery after falls in the elderly. In a landmark study published in the New England Journal of Medicine, the highest reported rates of mortality (death) and morbidity (injury) were those in people who were not found until 72 hours had passed (62%). But in those who received help within one hour, that rate fell to just 12%.
...when a fall happens, how quickly help arrives is critical...
Medical alert systems that incorporate passive fall detection technology, as well as active one-touch push-button response options, offer redundant layers of protection for falls and other medical or personal emergencies.
Double protection is especially important for seniors who live alone when considering the potential for medical emergencies such as heart attack, stroke, or fall-related head injuries; in such cases, the person may not be able to immediately affirmatively push a button or speak with a responding agent to summon help.
Neck-worn, pendant-style personal emergency response systems with fall detection features are passively monitored by trained agents and can dispatch emergency responders immediately, without the need to actively push a help button.
Many modern medical alert systems with fall detection are integrated with cellular networks and serve as standalone devices—a major step forward from early generations, which worked only at home, near landline-based hubs.
Such devices rely on GPS-based accelerometers that sense even tiny variations in motion, orientation (standing/sitting/lying down), and height. They account for sway, drop, and impact to distinguish between a device that has dropped by itself versus a person wearing a device who has fallen; when a fall is detected, an automatic alert is sent to personnel monitoring the device so help can be dispatched immediately. A help button can also be used to summon assistance at any time
Elderly fall prevention: Recognize, reduce, and mitigate common risk factors
Researchers have learned a great deal about how to prevent falls in the elderly. Ensuring older adults don’t sustain unnecessary injuries from falls is a shared responsibility. From caregiver and personal efforts to physician vigilance to community-based home modification and exercise programs and services, many evidence-based resources are available to help safeguard seniors from foreseeable fall hazards, both at home and away.
Mitigate medical risks
Many chronic health problems that tend to develop as we age can make falling more likely. Geriatricians (doctors who specialize in treating older adults) are trained in assessing and treating these conditions and more and can also help assess specific fall risks in individual patients. They can help caregivers and patients themselves come up with tailored plans to address elderly fall prevention.
Issues with the feet , like neuropathy, can cause numbness in the feet and affect balance. Regular foot care and well-fitting, stable shoes are the first step to addressing how to prevent falls in the elderly.
Muscle weakness and/or joint pain can cause difficulty walking as well as rising and lowering oneself from a sitting position, leading to falls to the floor as people attempt to move to or from beds or chairs. Physical therapy may restore some function and reduce fall risk during these transfers.
Heart disease, thyroid, and blood pressure issues may cause dizziness, lightheadedness, and unsteadiness, increasing the likelihood of falls.
Gait changes: As we grow older, the way in which we walk may change in subtle but important ways due to both neurological and musculoskeletal variations from “normal.” It is never normal for feet to drag on the ground or for toes to point inward; if these issues are observed, a visit to the doctor for assessment and possible physical therapy is indicated. Especially if there are notable deficits in gait, consistent use of appropriate assistive devices like canes and walkers can prevent a first fall and extend independence.
Medications: According to the CDC, many drugs can produce side effects that increase the risk of falls by increasing dizziness, disorientation, and impulsiveness. Best practice is to stop risky medications when possible, switch to alternatives that are safer, or reduce dosages of those that cannot be stopped. The riskiest drugs are psychoactive medications like sedatives and hypnotics (often prescribed to help older adults get to sleep), antidepressants, benzodiazepines (a class of anxiety drugs, like valium), opioid pain relievers, antipsychotics, and anticonvulsants. The risk goes up with alcohol consumption. Other medications, like muscle relaxants, antihistamines, blood pressure medications, and anticholinergics may also increase fall risk. Review all prescriptions and over-the-counter medications with a physician.
Vision and Hearing: While the role of reduced vision in falls is intuitive, it may be surprising that hearing loss is also a strong risk factor in falls in the elderly. In fact, older people with hearing loss are three times more likely to fall; for every ten decibels of hearing loss, researchers at Johns Hopkins found the chances of falling increase by a factor of 1.4. Up-to-date vision (glasses) and hearing aids are critical to preventing falls, as is wearing these devices at all times a person is moving around, both at home and away. These sensory aids help maintain full awareness of potential fall hazards in the environment.
Healthy lifestyle modifications to prevent falls
While not every older adult can prevent every fall through lifestyle modifications, there are some interventions that have been proven to help with elderly fall prevention for those who are capable of undertaking them.
Many of the following recommendations are recommended by consensus of such bodies as the National Institutes of Health, the National Alliance for Caregiving/National Council on Aging, and the U.S. Centers for Disease Control.
Physical conditioning
Balance and strength exercises are fall-prevention secret weapons in the battle to prevent falls. Maintaining core strength (abdominal and back muscles) as well as strength and flexibility in the leg, hip, ankle, and smaller muscles of the feet and toes can help to recover from unexpected wobbles that may otherwise turn into falls; regular exercise of these muscle groups after age 50 is critical to stave off the odds of taking a tumble. From simple exercises like marching in place, leg raises, and sit-to-stand to complex routines like Tai Chi, senior centers in many places offer safe, supervised, and modified routines—even for people who may be in wheelchairs.
Keep bones strong
Osteoporosis, or thinning, weakening bones, are another reason falls in the elderly cause more severe injuries than in younger people. To help keep bones from thinning as the years pass, doctors recommend several strategies:
Get regular weight-bearing exercise. This kind of exercise forces your body to lift weight (either your own body or other weights). Let gravity help keep your bones strong by walking, jogging, hiking, climbing stairs, or dancing regularly.
Maintain a healthy weight. Osteoporosis is one condition that strikes thin people more than heavier people, and it affects women far more than men. Seventy percent of osteoporosis patients, in fact, are women, and being underweight is a risk factor for osteoporosis. If a woman lost weight during the menopausal transition, she is more likely to develop osteoporosis. Doctors can scan bones to see if osteoporosis is present.
Stop smoking. Cigarette smoke negatively affects hormones in the body that bones desperately need to stay strong. Especially in the years after menopause, smoking compounds any bone loss that is already occurring. Limit or eliminate alcohol consumption. Heavy alcohol consumption has been linked with bone loss.
Get enough calcium and vitamin D. Both of these nutrients are critical for bone health. Doctors can test vitamin D levels to see how much is in the blood; the body manufactures its own when you go out in the sun, but if you aren’t getting enough, you may need a supplement. Calcium is contained in leafy greens, dairy products, nuts, and seeds, as well as supplements.
Home modifications to prevent falls
Stairs: Handrails on both sides (not just one) offer optimal stability.
Removing and modifying potential trip, slip, and fall hazards from inside and outside the home.
Floors: Bare is best. Throw rugs are trip hazards; the best course of action is to remove them. If they must be retained, use double-sided carpet tape to secure them the floor. Pets can also materialize underfoot quickly, sometimes without warning, creating a common cause of falls in the elderly; bells on collars can help older adults maintain awareness of a pet’s whereabouts and help keep track of a beloved companion’s whereabouts while walking in low-light areas or around blind corners.
Bathrooms: Nonskid, non-slip surfaces Rubber mats in showers and mats or carpet on floors help to eliminate slippery surfaces from under wet feet, while grab bars inside and outside the shower and near the toilet offer additional stability and leverage. Add non-skid strips to any hard surface that may get wet.
Stairs: Handrails on both sides (not just one) offer optimal stability. Use them, and consider a shoulder-or elbow-held handbasket, backpack, or cloth shopping bag to carry objects up and down stairs to keep both hands free to hold on to the railings.
Lighting: Vision, as previously noted, is a critical component of fall prevention. Install ample light everywhere, and don’t forget nightlights. Keep flashlights and light switches within easy reach. You may consider installing a “smart” lighting system that uses intelligent voice-activated home assistants (like Google Home and Amazon Echo) which allows control via smart switches by saying, “(Assistant), turn on the lights in the bedroom” before heading in,” or “Assistant, turn off all the lights” once safely tucked in bed.
Reaching: While it’s always tempting, never stand on a chair or a table to reach something that’s too high to reach for the ground. Reaching or grabbing sticks with “claws” are available affordably, or ask for help. It’s never worth risking a fall.
Outdoors: Be especially careful when it’s rainy, icy, or snowy outside. Use ample amounts of sand or salt during inclement weather to make slippery surfaces safer.
The risk of falls in the elderly can never be completely eliminated, and no fall detection system detects 100% of falls. But we know a great deal about how to prevent falls in the elderly, and fall risks can be it can be reduced and mitigated through coordinated efforts of older adults, their physicians, their pharmacists, and their family/caregivers.
Here’s more from Lively.
swipe for more
scroll or use your arrow keys for more
scroll for more
use your arrow keys for more



